How Can We Create Accurate Digital Twins of the Human Vasculature?
By Dr. Amanda Randles, Ph.D. — National Academy of Inventors Fellow & Alfred Winborne and Victoria Stover Mordecai Assistant Professor of Biomedical Sciences at Duke University
When someone is struggling with cardiovascular disease, they often need to become accustomed to invasive procedures as part of their treatment. In order to assess the severity of a blockage, cardiologists typically insert a guide wire in order to measure the pressure gradient in a patient’s circulatory system. An angioplasty may be required when significant blockages are found, which uses a balloon to open a blocked artery.
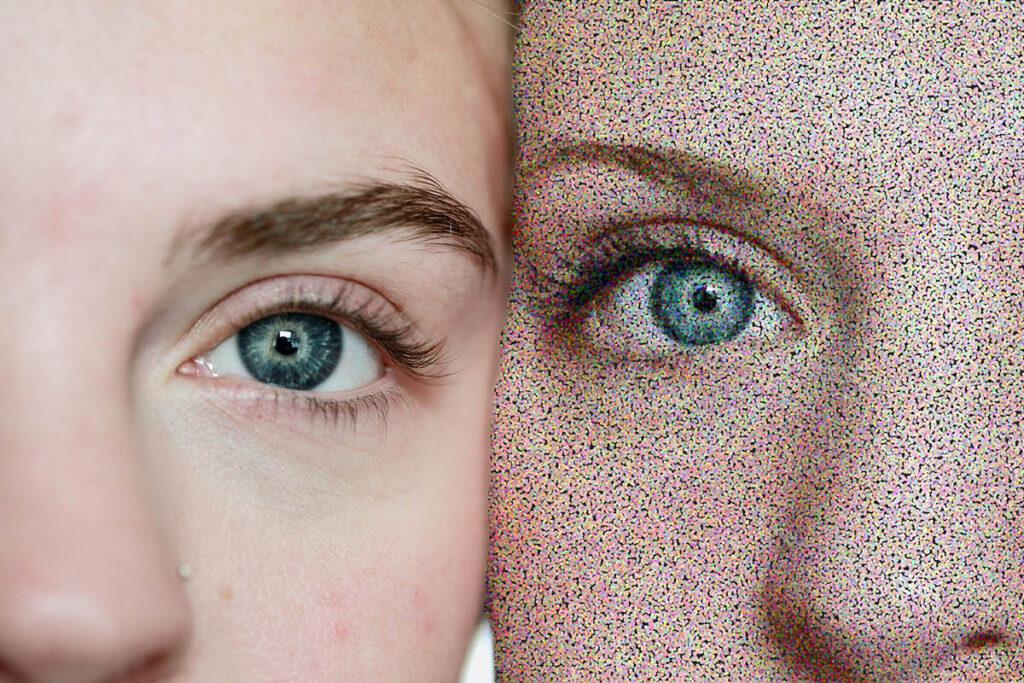
Traditional medicine has relied on these invasive procedures for years. However, digital simulation advancements allow doctors and scientists to create accurate digital twins of the human vascular system. Using high-fidelity, patient-specific simulations and machine learning, doctors may soon be able to measure pressure less invasively.
Creating personalized digital twins
A vascular digital twin is a computational model established to represent the 3-dimensional structure of a patient’s arteries and capture the behavior of their blood flow. By creating personalized, virtual models of someone’s coronary arteries, we can enable non-invasive diagnosis and provide a virtual testbed to assess a range of intervention options before the clinician ever steps into the operating room.
Creating a vascular twin starts with routine medical images such as those from MRI or CT scans. The primary goal is to create a set of images called a z-stack, giving medical professionals a look at a patient’s vessels across each plane. These images are then segmented to extract the 3D anatomical structure of that particular patient’s anatomy. This 3D structure is used to establish the digital twin. High-resolution, physics-based models can then be used to simulate blood flow in the derived anatomy. Other measures such as heart rate and cardiac output are used to further personalize the model. In our work, we use HARVEY, a computational fluid dynamics software customized for use on large-scale supercomputers, to simulate dynamic blood flow in the digital twin. Such models allow highly accurate, robust, and patient-specific measures of quantities such as the pressure gradient across a stenosis without the need for an invasive guidewire.
Improved diagnosis and treatment
The outlook for healthcare could be seen as bleak, with rising prices and a doctor shortage worsening year after year. Digital twins offer a promising method for addressing some concerns in the medical field by improving the process of diagnosis and treatment decisions. These virtual models even offer a means for secondary opinions or collaborative intervention planning in a distributed setting.
One example of the utility of digital twins is illustrated in our work with bifurcation lesions. By creating a personalized, digital twin of patients with bifurcation lesions, we could test out different treatment options for each patient and assess the resulting impact on blood flow virtually. For example, a key question in treating these lesions is determining if a stent is needed in both the primary and the side branch, or only in one or the other. Digital twins provide a platform for testing the effect of each of these options for that specific patient. Digital twins further allow for the testing of how each intervention would respond to different physiological states such as resting or exercise. All of this information can be used for a more informed and personalized treatment plan.
Assistance with the diagnosis and treatment of cardiovascular disease is not the only use of digital twins in the medical field, however. Along with vascular digital twins, we are using high-resolution models to create digital twins of microfluidic devices as well, thus allowing for high throughput measurements of quantities that are difficult to measure in a wet lab.
By augmenting in vitro models with digital twins, we are broadening the metrics that can be accessed and used to investigate cell properties. This is particularly interesting when characterizing cancer cells.
Timely solutions through virtual patient models
With disease, time is often of the essence. The time between diagnosis and effective treatment can be shortened by combining machine learning and physics-based modeling. This technology can help the healthcare industry reach better patient outcomes in a shorter amount of time.
Technology is revolutionizing the medical field. As advancements such as digital twin technology improve, medical providers will have access to more accurate diagnoses and a better view of treatment options and their possible outcomes.
As a result of our research, cardiologists and vascular surgeons can more accurately assess the effect of different interventions or stent placements as well as the impact of future physiological states in order to identify potential problems early on and improve surgical planning. The ability to create digital twins can reduce our reliance on invasive measurements and have a radically positive impact on the treatment process and patient outcomes.

Amanda E. Randles, Ph.D., is the Alfred Winborne Mordecai and Victoria Stover Mordecai Assistant Professor of Biomedical Sciences at Duke University. Randles has made significant contributions to the fields of high-performance computing and vascular modeling. Randles is the recipient of the NSF CAREER award, the ACM Grace Murray Hopper Award, IEEE-CS Technical Consortium on High-Performance Computing (TCHPC) Award, the NIH Director’s Early Independence Award, and the LLNL Lawrence Fellowship. Randles was also named to the World Economic Forum Young Scientist List and the MIT Technology Review World’s Top 35 Innovators under the Age of 35 list. She holds 120 U.S. patents and has published 71 peer-reviewed articles.